Global, regional and national burden of osteoarthritis 1990-2017: a systematic analysis of the Global Burden of Disease Study 2017.
Ann. Rheum. Dis. 2020; 79: 819-828
The global prevalence of rheumatoid arthritis: a meta-analysis based on a systematic review.
Rheumatol. Int. 2021; 41: 863-877
Discovery of an autoantibody signature for the early diagnosis of knee osteoarthritis: data from the Osteoarthritis Initiative.
Ann. Rheum. Dis. 2019; 78: 1699-1705
Pathogenesis of osteoarthritis: risk factors, regulatory pathways in chondrocytes, and experimental models.
Biology. 2020; 9: 194
Osteoarthritis: an ancient disease, an unsolved conundrum.
Int. Orthop. 2021; 45: 313-317
Current models for development of disease-modifying osteoarthritis drugs.
Tissue Eng. Part C Methods. 2021; 27: 124-138
Human mesenchymal stem cell-derived miniature joint system for disease modeling and drug testing.
Adv. Sci. 2022; 9e2105909
Restoring synovial homeostasis in rheumatoid arthritis by targeting fibroblast-like synoviocytes.
Nat. Rev. Rheumatol. 2020; 16: 316-333
Synovial cellular and molecular signatures stratify clinical response to csDMARD therapy and predict radiographic progression in early rheumatoid arthritis patients.
Ann. Rheum. Dis. 2019; 78: 761-772
Defining refractory rheumatoid arthritis.
Ann. Rheum. Dis. 2018; 77: 966-969
Clinical management of psoriatic arthritis.
Lancet. 2018; 391: 2285-2294
Skeletal infections: microbial pathogenesis, immunity and clinical management.
Nat. Rev. Microbiol. 2022; 20: 385-400
Generating 3D-cultured organoids for pre-clinical modeling and treatment of degenerative joint disease.
Signal Transduct. Target Ther. 2021; 6: 380
Adipose tissue is a critical regulator of osteoarthritis.
Proc. Natl. Acad. Sci. U. S. A. 2021; 118e2021096118
Targeting the gut microbiome to treat the osteoarthritis of obesity.
JCI Insight. 2018; 3e95997
Inhibition of TET1 prevents the development of osteoarthritis and reveals the 5hmC landscape that orchestrates pathogenesis.
Sci. Transl. Med. 2020; 12eaax2332
Nanoindentation modulus of murine cartilage: a sensitive indicator of the initiation and progression of post-traumatic osteoarthritis.
Osteoarthr. Cartil. 2017; 25: 108-117
Acute synovitis after trauma precedes and is associated with osteoarthritis onset and progression.
Int. J. Biol. Sci. 2020; 16: 970-980
Survey of clinical translation of cancer nanomedicines—lessons learned from successes and failures.
Acc. Chem. Res. 2019; 52: 2445-2461
Machine learning to predict anti-tumor necrosis factor drug responses of rheumatoid arthritis patients by integrating clinical and genetic markers.
Arthritis Rheum. 2019; 71: 1987-1996
Single-cell mass cytometry reveals cross-talk between inflammation-dampening and inflammation-amplifying cells in osteoarthritic cartilage.
Sci. Adv. 2020; 6eaay5352
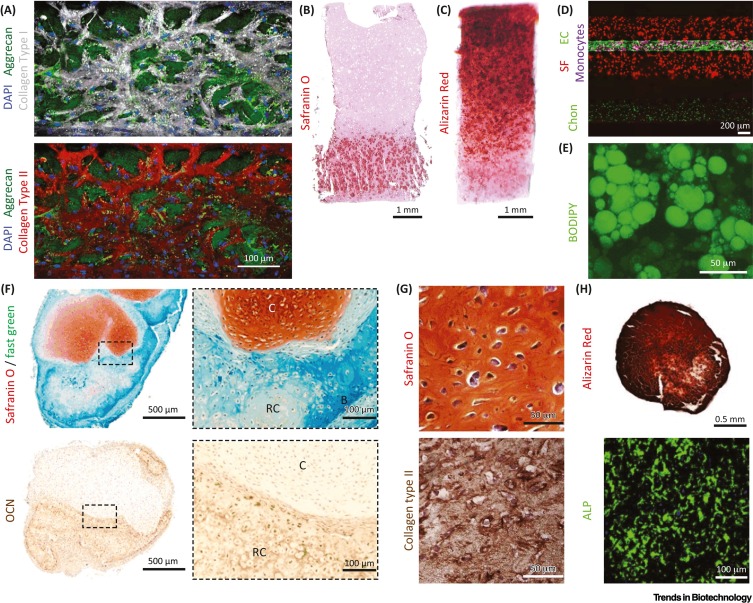
Engineering osteoarthritic cartilage model through differentiating senescent human mesenchymal stem cells for testing disease-modifying drugs.
Sci. China Life Sci. 2022; 65: 309-327
Modeling the human body on microfluidic chips.
Trends Biotechnol. 2021; 39: 838-852
Modeling human diseases with induced pluripotent stem cells: from 2D to 3D and beyond.
Development. 2018; 145dev156166
Organs-on-a-chip models for biological research.
Cell. 2021; 184: 4597-4611
Robotic fluidic coupling and interrogation of multiple vascularized organ chips.
Nat. Biomed. Eng. 2020; 4: 407-420
Recapitulating monocyte extravasation to the synovium in an organotypic microfluidic model of the articular joint.
Biofabrication. 2021; 13045001
Hyperphysiological compression of articular cartilage induces an osteoarthritic phenotype in a cartilage-on-a-chip model.
Nat. Biomed. Eng. 2019; 3: 545-557
Establishment of a human three-dimensional chip-based chondro-synovial coculture joint model for reciprocal cross talk studies in arthritis research.
Lab Chip. 2021; 21: 4128-4143
Microfluidic nutrient gradient-based three-dimensional chondrocyte culture-on-a-chip as an in vitro equine arthritis model.
Mater. Today Bio. 2019; 4100023
The pretreatment gut microbiome is associated with lack of response to methotrexate in new-onset rheumatoid arthritis.
Arthritis Rheum. 2021; 73: 931-942
Beyond polydimethylsiloxane: alternative materials for fabrication of organ-on-a-chip devices and microphysiological systems.
ACS Biomater. Sci. Eng. 2021; 7: 2880-2899
Progress in 3D bioprinting technology for tissue/organ regenerative engineering.
Biomaterials. 2020; 226119536
Functional 3D printing for microfluidic chips.
Adv. Mater. Technol. 2019; 41900275
Scalable fabrication of stretchable, dual channel, microfluidic organ chips.
J. Vis. Exp. 2018; 140e58151
Monitoring tissue-level remodelling during inflammatory arthritis using a three-dimensional synovium-on-a-chip with non-invasive light scattering biosensing.
Lab Chip. 2020; 20: 1461-1471
Bioprinting of 3D convoluted renal proximal tubules on perfusable chips.
Sci. Rep. 2016; 6: 34845
Stem cell-based microphysiological osteochondral system to model tissue response to interleukin-1β.
Mol. Pharm. 2014; 11: 2203-2212
Osteochondral tissue chip derived from iPSCs: modeling OA pathologies and testing drugs.
Front. Bioeng. Biotechnol. 2019; 7: 411
Combinatorial screening of biochemical and physical signals for phenotypic regulation of stem cell-based cartilage tissue engineering.
Sci. Adv. 2020; 6eaaz5913
Integrating organs-on-chips: multiplexing, scaling, vascularization, and innervation.
Trends Biotechnol. 2020; 38: 99-112
Cartilage-on-a-chip to aid OA drug development.
Nat. Rev. Rheumatol. 2019; 15: 511
Pneumatic microfluidic cell compression device for high-throughput study of chondrocyte mechanobiology.
Lab Chip. 2018; 18: 2077-2086
A high-throughput mechanical activator for cartilage engineering enables rapid screening of in vitro response of tissue models to physiological and supra-physiological loads.
Cells Tissues Organs. 2021; 211: 54-72
A 3D human adipose tissue model within a microfluidic device.
Lab Chip. 2021; 21: 435-446
Mechanically stimulated osteochondral organ culture for evaluation of biomaterials in cartilage repair studies.
Acta Biomater. 2018; 81: 256-266
TRPV4 activation enhances compressive properties and glycosaminoglycan deposition of equine neocartilage sheets.
Osteoarthr. Cartil. Open. 2022; 4100263
Synergy between Piezo1 and Piezo2 channels confers high-strain mechanosensitivity to articular cartilage.
Proc. Natl. Acad. Sci. U.S.A. 2014; 111: E5114-E5122
Inflammatory signaling sensitizes Piezo1 mechanotransduction in articular chondrocytes as a pathogenic feed-forward mechanism in osteoarthritis.
Proc. Natl. Acad. Sci. U.S.A. 2021; 118e2001611118
Macrophage effects on mesenchymal stem cell osteogenesis in a three-dimensional in vitro bone model.
Tissue Eng. Part A. 2020; 26: 1099-1111
Adipose tissue-derived stem cells retain their adipocyte differentiation potential in three-dimensional hydrogels and bioreactors.
Biomolecules. 2020; 10: 1070
Macrophages modulate the function of MSC- and iPSC-derived fibroblasts in the presence of polyethylene particles.
Int. J. Mol. Sci. 2021; 22: 12837
Modulation of inflammation by anti-TNF α mAb-dendrimer nanoparticles loaded in tyramine-modified gellan gum hydrogels in a cartilage-on-a-chip model.
J. Mater. Chem. B. 2021; 9: 4211-4218
The effects of macrophage phenotype on osteogenic differentiation of MSCs in the presence of polyethylene particles.
Biomedicines. 2021; 9: 499
A microfluidic chip-based co-culture of fibroblast-like synoviocytes with osteoblasts and osteoclasts to test bone erosion and drug evaluation.
R. Soc. Open Sci. 2018; 5180528
Osteoarthritis year in review: genetics, genomics, epigenetics.
Osteoarthr. Cartil. 2021; 29: 151-160
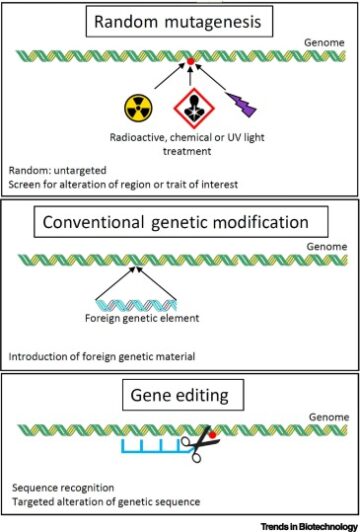
Generation of a heterozygous COL2A1 (p.G1113C) hypochondrogenesis mutation iPSC line, MCRIi019-A-7, using CRISPR/Cas9 gene editing.
Stem Cell Res. 2021; 56102515
Capturing essential physiological aspects of interacting cartilage and bone tissue with osteoarthritis pathophysiology: a human osteochondral unit-on-a-chip model.
Adv. Mater. Technol. 2022; ()
Development of a human osteochondral construct on a microfluidic chip–to advance functional studies of osteoarthritis risk genes.
Osteoarthr. Cartil. 2021; 29: S108-S109
Gut-on-a-chip: mimicking and monitoring the human intestine.
Biosens. Bioelectron. 2021; 181113156
Single-cell RNA-seq reveals transcriptomic heterogeneity and post-traumatic osteoarthritis-associated early molecular changes in mouse articular chondrocytes.
Cells. 2021; 10: 1462
Mapping signalling perturbations in myocardial fibrosis via the integrative phosphoproteomic profiling of tissue from diverse sources.
Nat. Biomed. Eng. 2020; 4: 889-900
Gene therapy for follistatin mitigates systemic metabolic inflammation and post-traumatic arthritis in high-fat diet-induced obesity.
Sci. Adv. 2020; 6eaaz7492
Characterization of synovial fluid metabolomic phenotypes of cartilage morphological changes associated with osteoarthritis.
Osteoarthr. Cartil. 2019; 27: 1174-1184
Individual cartilage aggrecan macromolecules and their constituent glycosaminoglycans visualized via atomic force microscopy.
J. Struct. Biol. 2003; 143: 242-257
Exosomes in the pathogenesis, progression, and treatment of osteoarthritis.
Bioengineering. 2022; 9: 99
Personalised organs-on-chips: functional testing for precision medicine.
Lab Chip. 2019; 19: 198-205
Microenvironment in subchondral bone: predominant regulator for the treatment of osteoarthritis.
Ann. Rheum. Dis. 2021; 80: 413-422
Microfluidic vascularized bone tissue model with hydroxyapatite-incorporated extracellular matrix.
Lab Chip. 2015; 15: 3984-3988
An in vitro chondro-osteo-vascular triphasic model of the osteochondral complex.
Biomaterials. 2021; 272120773
Human bone perivascular niche-on-a-chip for studying metastatic colonization.
Proc. Natl. Acad. Sci. U.S.A. 2018; 115: 1256-1261
Buoyancy-driven gradients for biomaterial fabrication and tissue engineering.
Adv. Mater. 2019; 311900291
Biomimetic gradient hydrogels for tissue engineering.
Can. J. Chem. Eng. 2010; 88: 899-911
Low-grade inflammation as a key mediator of the pathogenesis of osteoarthritis.
Nat. Rev. Rheumatol. 2016; 12: 580-592
WAT-on-a-chip: a physiologically relevant microfluidic system incorporating white adipose tissue.
Lab Chip. 2017; 17: 1645-1654
Establishment and characterization of a primary murine adipose tissue-chip.
Biotechnol. Bioeng. 2018; 115: 1979-1987
Bone marrow mesenchymal stem cells: aging and tissue engineering applications to enhance bone healing.
Biomaterials. 2019; 203: 96-110
Graphene oxide-functionalized nanocomposites promote osteogenesis of human mesenchymal stem cells via enhancement of BMP-SMAD1/5 signaling pathway.
Biomaterials. 2021; 277121082
Induced pluripotent stem cells: past, present, and future.
Cell Stem Cell. 2012; 10: 678-684
Stiffness matters: fine-tuned hydrogel elasticity alters chondrogenic redifferentiation.
Front. Bioeng. Biotechnol. 2020; 8: 373
A novel organ-chip system emulates three-dimensional architecture of the human epithelia and the mechanical forces acting on it.
Biomaterials. 2021; 275120957
Brain organoids: advances, applications and challenges.
Development. 2019; 146dev166074
Generation of lung organoids from human pluripotent stem cells in vitro.
Nat. Protoc. 2019; 14: 518-540
Evaluation of variability in human kidney organoids.
Nat. Methods. 2019; 16: 79-87
Culture and establishment of self-renewing human and mouse adult liver and pancreas 3D organoids and their genetic manipulation.
Nat. Protoc. 2016; 11: 1724-1743
Intestinal organoid cocultures with microbes.
Nat. Protoc. 2021; 16: 4633-4649
Vascularized adipocyte organoid model using isolated human microvessel fragments.
Biofabrication. 2021; 13035022
The horizon of bone organoid: A perspective on construction and application.
Bioact. Mater. 2022; 18: 15-25
Robust bone regeneration through endochondral ossification of human mesenchymal stem cells within their own extracellular matrix.
Biomaterials. 2019; 218119336
Developmentally engineered callus organoid bioassemblies exhibit predictive in vivo long bone healing.
Adv. Sci. 2020; 71902295
Patterned, organoid-based cartilaginous implants exhibit zone specific functionality forming osteochondral-like tissues in vivo.
Biomaterials. 2021; 273120820
Formation of osteochondral organoids from murine induced pluripotent stem cells.
Tissue Eng. Part A. 2021; 27: 1099-1109
Scaffold-free generation of uniform adipose spheroids for metabolism research and drug discovery.
Sci. Rep. 2018; 8: 523
Synergistic engineering: organoids meet organs-on-a-chip.
Cell Stem Cell. 2017; 21: 297-300
One-step fabrication of an organ-on-a-chip with spatial heterogeneity using a 3D bioprinting technology.
Lab Chip. 2016; 16: 2618-2625
Botanical-inspired 4D printing of hydrogel at the microscale.
Adv. Funct. Mater. 2020; 301907377
- SEO Powered Content & PR Distribution. Get Amplified Today.
- Platoblockchain. Web3 Metaverse Intelligence. Knowledge Amplified. Access Here.
- Source: https://www.cell.com/trends/biotechnology/fulltext/S0167-7799(22)00193-7?rss=yes
- 1
- 2017
- 2D
- 3d
- 3D Printing
- a
- Activation
- Adult
- advance
- advances
- After
- Aging
- Aid
- alternative
- analysis
- Ancient
- and
- Application
- applications
- architecture
- aspects
- associated
- authors
- based
- between
- Beyond
- Biomaterials
- body
- BONE
- Bosch
- burden
- Cancer
- Cells
- challenges
- Changes
- Channel
- channels
- China
- chip
- Chips
- Clinical
- complex
- constituent
- construct
- construction
- critical
- Cross
- Culture
- data
- Den
- Derived
- Development
- device
- Devices
- discovery
- Disease
- diseases
- diverse
- drug
- drug development
- drug discovery
- drug testing
- Drugs
- during
- Early
- effects
- enables
- Engineering
- Enhances
- epigenetics
- essential
- establishment
- evaluation
- exhibit
- factors
- Force
- Forces
- from
- function
- functional
- functionality
- future
- gene editing
- generation
- Genetics
- genomics
- Global
- gradients
- Hall
- horizon
- HTTPS
- human
- immunity
- in
- incorporating
- Indicator
- Infections
- inflammation
- Initiative
- insight
- Integrating
- interacting
- isolated
- IT
- Key
- kidney
- Lack
- landscape
- learned
- learning
- Life
- light
- Line
- List
- Liver
- loads
- Long
- management
- Manipulation
- Mass
- materials
- Matrix
- Matters
- mechanical
- mechanism
- medicine
- Meet
- methods
- Microbiome
- Microscopy
- model
- modeling
- models
- MOL
- molecular
- monitoring
- multiple
- Mutation
- National
- novel
- Obesity
- open
- own
- part
- past
- patients
- perspective
- phenotype
- physical
- plato
- Plato Data Intelligence
- PlatoData
- potential
- Precision
- predict
- presence
- present
- primary
- profiling
- Progress
- progression
- promote
- properties
- rapid
- regenerative
- regional
- Regulation
- regulator
- regulatory
- relevant
- repair
- research
- response
- Reveals
- review
- Risk
- risk factors
- scaling
- SCI
- screening
- sensitive
- signals
- Signatures
- Sources
- Spatial
- specific
- Stem
- stem cells
- studies
- Study
- Studying
- system
- systemic
- Systems
- Talk
- Target
- targeting
- Technology
- test
- Testing
- The
- their
- therapy
- three-dimensional
- Through
- tissues
- to
- today
- Translation
- treat
- treatment
- via
- vivo
- W
- white
- within
- X
- year
- zephyrnet