The last few years have been a strain on nearly everyone, with routines disrupted, social interactions curtailed, and stress and anxiety running high.
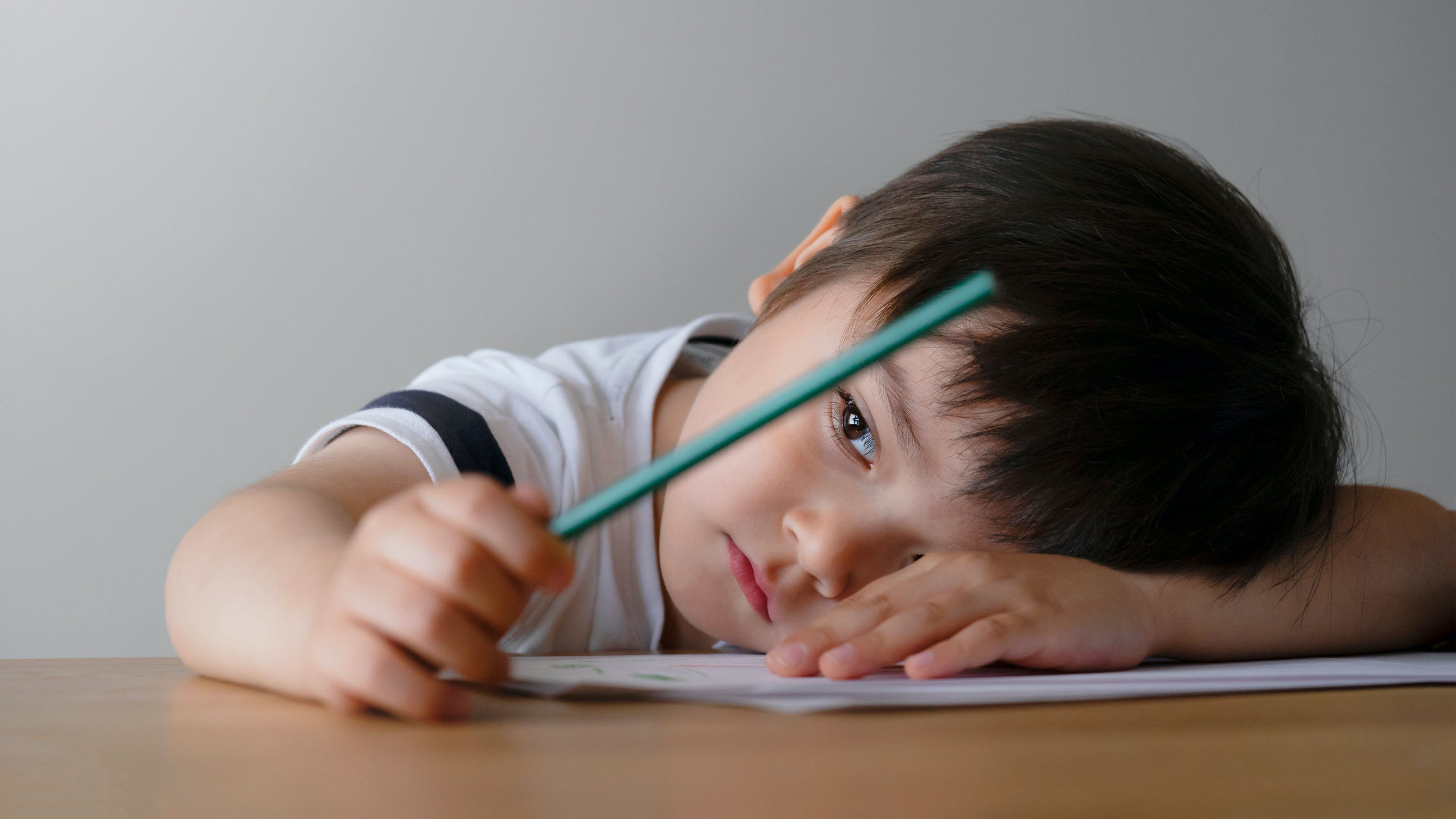
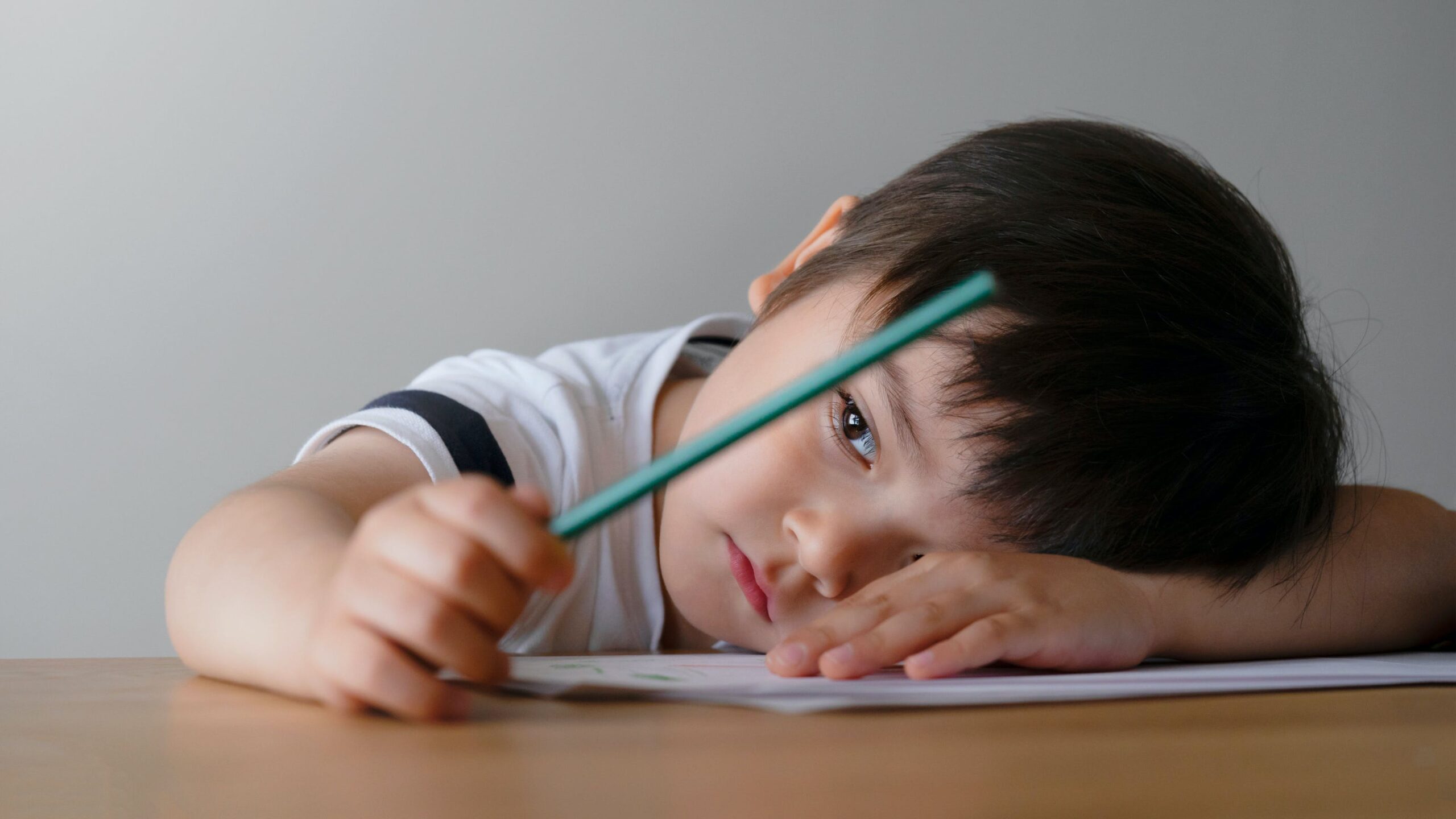
There’s been much written and discussed about how those challenges have impacted students in K-12 schools and colleges — how they're suffering in the wake of the pandemic and experiencing alarmingly high rates of mental health concerns. But what about kids who are even younger — infants, toddlers and preschool-aged children who also lived through the pandemic and are not immune to the stressors that it caused?
Those kids — yes, even babies — have suffered too, experts say. And given how foundational this period of their lives is for future outcomes and development, it’s especially urgent that the mental health and well-being of infants and young children be addressed early.
“We like to say that the social-emotional health [and] mental health of little ones is all our jobs — anyone who touches the life of a child — because of the fact that brain development is so rapid in the prenatal-to-3 space of life,” says Meghan Schmelzer, senior manager of infant and early childhood mental health at the nonprofit Zero to Three. “We can see the huge consequences when things don’t go right in the first three years of life.”
While this idea is supported by research, it is not yet widely known, accepted or understood among families and other adults.
When Angela Keyes, an associate professor of psychiatry at Tulane University and co-director of an infant and early childhood mental health consultation program, tells people she is an infant mental health specialist, she says they often ask her, incredulously, “Infants can have mental health struggles?”
When babies and young children experience hardship — poverty, violence, food insecurity, neglect and any number of other traumas — many adults brush it off, saying, Oh, but kids are resilient, or maybe, They’re too young to remember this.
“Babies remember,” Schmelzer corrects. “They just remember it differently. We remember in our brains, and they remember in their bodies.”
And while kids are remarkably resilient, they’re also vulnerable, she adds. An estimated 10 to 16 percent of young kids experience mental health issues, including PTSD and anxiety, Schmelzer says, referencing data from Think Babies and the Centers for Disease Control and Prevention. For kids in poverty, the rate is more like 22 percent.
It’s not impossible for babies and toddlers to overcome these challenges — “That’s not a sentence for them,” Schmelzer says — but it takes a lot of love, support and intervention.
What Mental Health Issues Look Like in Little Kids
Without intervention and a nurturing environment, the impacts of trauma and stress can be immediate and long-lasting, explains Nancy Kelly, the mental health promotion branch chief at the federal government’s Substance Abuse and Mental Health Services Administration (SAMHSA).
Those consequences can present in a lot of different forms, Kelly says. Some children may struggle to form attachments. They don’t want to be held, perhaps. Or they don’t want to be touched. Some children may act out. Babies may reject food or cry inconsolably. Kids who may have already been toilet trained could revert to wetting the bed or wetting themselves. Some will develop separation anxiety.
These behaviors are not wholly unlike the behaviors of an adult who is experiencing trauma or mental health challenges, Kelly points out. Adults may cry or lose their appetites. They might spend excessive amounts of time in bed, curled up in a fetal position. They may become emotionally detached from others or, the opposite, need constant connection, reassurance and attention.
Babies and young children may not be able to communicate verbally what is going on with them, but they are still communicating, Schmelzer notes.
“Behaviors that are ‘challenging’ — that’s a red flag. It’s a signal to us,” she says.
For educators and caregivers, Keyes offers a couple of examples of how children’s behaviors can signal to adults that something is up.
A little boy is new to a child care program, and each day, after his parents drop him off, he becomes distraught. Later, the teachers in his program learn that the boy had recently overheard a heated argument between his parents that made him scared. He didn’t want to be separated from them.
A toddler has become withdrawn, refusing to eat or play or participate, sometimes hiding under the table in her program. Her teachers learn that the girl has recently been placed in foster care, removed from her home and her parents. She’s experiencing attachment disruption, and everything around her — from the place where she sleeps to the people she sees to the food she eats — is unfamiliar.
What Keyes is trying to illustrate is that, while it may take some investigating on the part of the child’s caregivers, the explanations behind children’s behaviors are often knowable, she says. She often asks herself, “What is this child trying to tell me through their behavior?” The question is a prompt to find out what happened to this child instead of framing it as what is wrong with this child.
Another critical but often untapped resource in understanding what children’s behaviors are communicating? Their parents, Keyes says.
Many families would be able to tell the child’s teachers things like how a child has been eating, whether they slept well the night before, if they’re coming down with an illness, if they’re teething and whether something troubling is happening at home. But they aren’t always asked those questions. And during the pandemic, when parents were not allowed to enter the building of their child care program, let alone their child’s individual classroom, that communication channel was cut off.
Even now, Keyes says, many programs still limit who can enter certain spaces.
“We lost that ability to connect with parents, to build relationships with parents,” she says. “That has impacted our ability to get information about how a child is doing and what’s happening in their home.”
The Link Between Caregivers and Kids
Often, how a child is doing depends heavily on how their parents and caregivers are doing.
“Babies don’t live alone,” Schmelzer says. “Their caregivers’ mental health is inextricably tied to their mental health.”
And caregivers’ mental health — that of both parents and early childhood educators — has declined considerably since the pandemic began three years ago.
Recent research from the Yale Child Study Center found that, a few months into the pandemic, about 46 percent of child care providers had potentially diagnosable levels of depression and 67 percent reported moderate to high stress levels.
Surveys conducted by the RAPID-EC project based out of the University of Oregon found in fall 2022 that about 42 percent of families of young children are struggling with well-being and emotional distress, which includes anxiety, depression and loneliness.
“The mental health of adults impacts the mental health of kids,” Schmelzer explains. “If parents and families are more stressed, that’s going to impact the mental health and ultimately the development of their kids.”
So the pandemic’s toll on adults is affecting children. But children also experienced their own direct impacts from the pandemic.
More than 200,000 children in the U.S. have lost a parent or primary caregiver to COVID-19, and many of those children have been orphaned — a loss that will define the rest of their lives.
Over the last three years, amid program closures and quarantines, children also missed out on important opportunities to practice the skills that will set them up for a lifetime of future success: emotion regulation, tolerance for sharing and taking turns, following a schedule, transitioning to different activities.
“It was hard to get into a rhythm,” Keyes recalls of the pandemic. “Children were home with parents and not with other children. … Now what we’re seeing is a lot of mental health struggles for our youngest kiddos.”
Early Intervention
Fortunately, there are ways to help. Access to support and services for infant and early childhood mental health exists on a continuum, Schmelzer of Zero to Three explains: promotion, prevention, assessment, diagnosis and treatment.
Mental health consultation helps to address promotion and prevention by placing a mental health professional in a setting that serves infants, toddlers and young children. These settings include child care centers and in-home child care programs, pediatrician offices and families’ homes.
During mental health consultation, mental health professionals will often work with the adults who are caring for children to understand and improve policies, practices and the overall learning environment to create a more nurturing and positive space for kids, Schmelzer says.
Keyes, the psychiatry professor at Tulane, is part of a team of about 20 mental health consultants who go into child care programs across Louisiana, through a contract with the state education department. Consultants visit larger programs once a week for about four to eight hours and smaller programs every other week.
During these consultations, Keyes may observe classroom activities, work closely with the director and talk with teachers to understand how the program and individual classrooms are operating. Then she may suggest some tweaks, modeling for them different classroom strategies and behavior management.
“It’s not as rare as it used to be,” Keyes says of mental health consultation in early childhood. “More states are bringing it in. But it varies widely.”
Some places, such as Colorado, Illinois and Ohio, offer mental health consultation statewide. But Schmelzer notes that there’s an important distinction between offering it and actually having sufficient resources to meet demand. She previously was involved in infant mental health consultation in Michigan, where the program was technically statewide but had nowhere near enough position to provide services universally.
In her current position, Schmelzer is working with 13 states on how they can use American Rescue Plan dollars to expand their mental health work in early childhood.
“There has been a surge, in the last few years, of the understanding about mental health consultation as a support,” Schmelzer says.
And given the links between caregivers’ mental health and kids’ mental health, many programs are aimed at supporting both in concert. That includes the various infant and early childhood mental health programs offered by the U.S. Department of Health and Human Services, through SAMHSA, according to Kelly.
She thinks of it as similar to putting on your own oxygen mask on the airplane before helping a child with theirs — caregivers can’t really help kids with their mental health challenges until they’ve addressed their own.
“The whole portfolio is really around creating strong caregiving relationships and nurturing environments,” Kelly says, “so children can thrive.”
- SEO Powered Content & PR Distribution. Get Amplified Today.
- Platoblockchain. Web3 Metaverse Intelligence. Knowledge Amplified. Access Here.
- Source: https://www.edsurge.com/news/2023-02-28-who-s-looking-out-for-the-mental-health-of-infants-and-toddlers
- 000
- 10
- 2022
- 67
- a
- ability
- Able
- About
- abuse
- access
- According
- across
- Act
- activities
- actually
- address
- Adds
- administration
- Adult
- adults
- affecting
- After
- Airplane
- All
- alone
- already
- always
- American
- Amid
- among
- amounts
- and
- Anxiety
- anyone
- argument
- around
- assessment
- Associate
- attention
- based
- because
- become
- becomes
- before
- behind
- between
- Brain
- brains
- Branch
- Bringing
- build
- Building
- care
- caused
- CDC
- Center
- Centers
- certain
- challenges
- Channel
- chief
- child
- Children
- closely
- Colleges
- Colorado
- coming
- communicate
- communicating
- Communication
- concert
- conducted
- Connect
- connection
- Consequences
- constant
- consultants
- consultation
- consultations
- Continuum
- contract
- control
- could
- Couple
- COVID-19
- create
- Creating
- critical
- Current
- Cut
- data
- day
- Demand
- Department
- depends
- depression
- develop
- Development
- different
- different forms
- direct
- Director
- discussed
- Disease
- Disruption
- distress
- doing
- dollars
- Dont
- down
- Drop
- during
- each
- Early
- eat
- Education
- educators
- enough
- Enter
- Environment
- environments
- especially
- estimated
- Even
- Every
- everyone
- everything
- examples
- exists
- Expand
- experience
- experienced
- experiencing
- experts
- Explains
- Fall
- families
- Federal
- few
- Find
- First
- following
- food
- form
- forms
- Foster
- found
- from
- future
- get
- Girl
- given
- Go
- going
- happened
- Happening
- Hard
- hardship
- having
- Health
- health services
- heavily
- Held
- help
- helping
- helps
- High
- Home
- Homes
- HOURS
- How
- HTTPS
- huge
- human
- idea
- illinois
- illness
- immediate
- Impact
- impacted
- Impacts
- important
- impossible
- improve
- in
- include
- includes
- Including
- individual
- information
- instead
- interactions
- intervention
- involved
- issues
- IT
- Jobs
- kids
- known
- larger
- Last
- LEARN
- learning
- levels
- Life
- lifetime
- LIMIT
- LINK
- links
- little
- live
- Lives
- Loneliness
- Look
- look like
- looking
- lose
- loss
- Lot
- Louisiana
- love
- made
- management
- manager
- many
- mask
- Meet
- mental
- Mental health
- Michigan
- might
- modeling
- months
- more
- Near
- nearly
- Need
- New
- night
- Nonprofit
- Notes
- number
- observe
- offer
- offered
- offering
- Offers
- offices
- Ohio
- operating
- opportunities
- opposite
- Oregon
- Other
- Others
- overall
- Overcome
- own
- Oxygen
- pandemic
- parents
- part
- participate
- People
- percent
- perhaps
- period
- Place
- Places
- placing
- plan
- plato
- Plato Data Intelligence
- PlatoData
- Play
- points
- policies
- portfolio
- position
- positive
- potentially
- Poverty
- practice
- practices
- present
- Prevention
- previously
- primary
- professional
- professionals
- Professor
- Program
- Programs
- project
- promotion
- provide
- provide services
- providers
- PTSD
- Putting
- Quarantines
- question
- Questions
- rapid
- RARE
- Rate
- Rates
- RE
- reassurance
- recently
- Red
- refusing
- Regulation
- Relationships
- remember
- Removed
- Reported
- rescue
- research
- resilient
- resource
- Resources
- REST
- revert
- running
- says
- scared
- schedule
- Schools
- seeing
- sees
- senior
- sentence
- serves
- Services
- set
- setting
- settings
- sharing
- Signal
- similar
- since
- skills
- smaller
- So
- Social
- some
- something
- Space
- spaces
- specialist
- spend
- State
- States
- Still
- strategies
- stress
- strong
- Struggle
- Struggles
- Struggling
- Students
- Study
- substance
- success
- such
- sufficient
- support
- Supported
- Supporting
- surge
- table
- Take
- takes
- taking
- Talk
- teachers
- team
- tells
- The
- The State
- their
- themselves
- things
- Thinks
- three
- Thrive
- Through
- Tied
- time
- to
- Toilet
- tolerance
- too
- touched
- trained
- transitioning
- treatment
- troubling
- u.s.
- Ultimately
- under
- understand
- understanding
- understood
- unfamiliar
- university
- untapped
- urgent
- us
- use
- various
- VOX
- Vulnerable
- Wake
- ways
- week
- What
- What is
- whether
- which
- while
- WHO
- wholly
- widely
- will
- Work
- working
- would
- written
- Wrong
- years
- young
- Younger
- Youngest
- Your
- zephyrnet
- zero









![Project Tomorrow Research: Parents' Views on District Provided Devices and Connectivity [Infographic] - EdSurge News](https://platoaistream.com/wp-content/uploads/2023/08/project-tomorrow-research-parents-views-on-district-provided-devices-and-connectivity-infographic-edsurge-news-52x300.png)