Introduction
It’s been estimated that the human body contains about 60,000 miles of blood vessels. The heart has to pump blood through every inch of them unceasingly to meet the body’s bottomless needs for oxygen and nutrients. But because the heart has its own needs too, some of those vessels form a filigree of coronary arteries that laces through the cardiac muscle. If something goes wrong with those arteries — as when a cholesterol plaque growing on their lining ruptures and blocks them — sections of the heart can malfunction and sometimes die. Even if someone survives such a heart attack, the resulting scar tissue can permanently impair the heart’s strength and efficiency. Understanding the growth, development and maintenance of coronary arteries is therefore crucial for reducing the toll of heart disease.
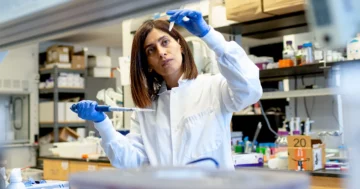
Kristy Red Horse, an associate professor of biology at Stanford University and a member of the school’s Institute for Stem Cell Biology and Regenerative Medicine, has become a leader in the pursuit of that understanding. She has published groundbreaking studies on the origins of blood vessels in the hearts of mammals. The hope is that what she and her colleagues have learned about the growth of those vessels during fetal development could help rescue the heart after a heart attack.
In 2021, the Howard Hughes Medical Institute (HHMI) selected Red Horse for its prestigious Investigator Program, perhaps the richest prize in biology. Her Stanford laboratory will receive $9 million over a seven-year period to fund its research. The grant has been a boon to her science, but it has also created opportunities for Red Horse, who is of Cherokee descent, to double down on her support and advocacy for Native American scientists.
Quanta spoke with Red Horse last summer while she was visiting New York and later in video calls. The interviews have been condensed and edited for clarity.
In 2021, you were appointed as an HHMI Investigator for your research connected to the regeneration and repair of heart tissue. Can you please describe those studies?
That work centered on the heart and its blood vessels — their embryonic development and biological functions. Specifically, we’ve been focusing on how the cardiovascular system is formed and on specialized blood vessels called collateral arteries. These can be found in animals like mice and guinea pigs, and also some (but not all) humans.
Usually, collaterals form in response to a heart injury. When there’s damage to the coronary vasculature that brings blood to the heart muscle, collateral arteries make new connections in the injured area. In our research, we’ve seen that when coronary arteries become blocked, the collaterals can in some instances become an alternate pathway for blood flow to the heart muscle. They can act as natural bypasses.
Introduction
Could this be important for treating heart disease?
Yes, we hope that understanding collaterals might be key to a new type of regenerative therapy. What we’ve been looking at is how this type of blood vessel develops and whether, at some point in the future, inducing them to grow might be an effective therapy for people with blocked coronary arteries.
Heart attacks occur when the blood can’t go around a vascular blockage. Like strokes, they happen in the blood vessels. When the heart muscle is denied oxygen and nutrients, heart tissue dies. That’s why, in many instances, heart failure ensues. But what if we could find a way to generate new coronary arteries to bring nutrients to the heart? Might we prevent heart muscle death?
One of our big discoveries is that collaterals in the mammalian heart form easily just after birth — that is, in neonates, or newborns. This may be one reason why, in the rare cases of newborns having heart attacks, they can heal quickly. Their collaterals extend out of regular arteries and migrate toward an injury. But in adults, the process is less efficient.
How far have you gotten in your research?
Well, among things we’ve discovered is that these collateral arteries are made from the same types of cells as regular arteries.
Prior to our research, it was thought that new collaterals were only transformed capillaries — small, preexisting blood vessels that were being expanded and remodeled. That does happen, but collaterals can in fact also grow out anew from existing arteries.
In experiments with young mice, we created blood vessel blockages and heart attacks. That set off the development of new collaterals in the animals. The collaterals originated in the lining of regular arteries and then grew to where the damage occurred.
Later, we identified a protein, CXCL12, that activates collateral artery formation. We used it to reawaken the process in adult mice. Right now, we are searching for other proteins involved in this process. We next intend to learn why some humans have collaterals and others don’t.
Prominent scientists say that you and your colleagues have transformed coronary research. Your Stanford colleague Irving Weissman, the legendary stem cell researcher, told me, “Kristy has given us an entirely different way to look at blood vessels.”
I think he’s speaking of my postdoctoral work with Mark Krasnow. Till we published it in 2010, the conventional wisdom was that the coronary arteries were made from the cellular covering of the embryonic heart — tissue called the epicardium. In our experiments, though, we saw that they instead originate from two other sources: a vein beside the heart called the sinus venosus and the inner lining of the heart, the endocardium.
To discover this, I used new techniques for looking at heart development. The old way to get a window on what was happening was to make tissue sections, very thin slices of tissue that looked at little pieces of the heart one at a time. I brought in this idea to look at the entire organ at once. This approach revealed the origins of the coronary arteries because you could see where they were emerging from, and you could see physical connections that you couldn’t when you just sliced and diced tissue.
Moreover, Irv Weissman had created this novel technique for looking at individual cells. He’d made this lineage of specially modified mice in which we could label just a few cells in an area with a color. After marking the cells, you could see during development where the cells and their offspring migrated to. We used that to help us confirm that the coronary arteries came from a vein and the inner lining of the heart.
It must have been exciting to discover something so unexpected.
Absolutely. It was thrilling when we actually saw that there were these two different progenitors of the coronaries and we saw them come from the inside of the heart chamber.
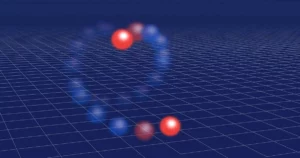
You could see the inside of the heart kind of spit out these little balls. They popped out in these circles, as if they were tiny beach balls. And then they spread out. I was like, “What? Wow!” It was not how we anticipated blood vessels growing.
What’s also fascinating is that if you look at the individual cells early in the development of the coronaries, you can tell which ones came from the vein and which ones came from the heart lining. They carry different molecular signatures. But by the time the coronaries have matured, the cells all seem to converge on the exact same form, down to the level of identical gene expression. So they respond to cardiac injuries in the same way.
Why would nature have two different ways of making the same cells? That seems oddly wasteful.
There are at least a couple of ideas about that. One possibility is that because coronary arteries are so vital to an animal’s health, this gives us a backup way to grow them. In experiments, we’ve shown that if the growth of coronary vessels from the sinus venosus is interrupted, the vessels from the endocardium expand to fill the gap.
Having two sources may also help the network of coronary arteries grow faster. More starting material means faster expansion. The optimum growth of the vessels seems to be important for making sure that the heart muscle itself develops quickly into a tight, compact form, which the heart needs to beat efficiently.
Introduction
The Nature paper in which you, Weissman and Krasnow described the two sources of coronary arteries was a bombshell. Later, did you wonder if you’d ever top that?
It was a flashy thing, that finding. And when you do a flashy thing, a lot of people discuss it and wonder if it is actually true. What I did for the next few years in my lab was to develop new tools so that we could hammer that out. We showed that the flashy paper was actually true, and I next zeroed in on proving the details.
That’s one of the things that I think is special about my lab. We don’t just go for the splashy publication and then move on. We take the time to describe the biology, and we go through a real effort to make sure we’re correct.
The HHMI Investigator Program is one of the richest honors in biological research. You were promised $9 million over seven years for that. Did it change your life?
It changed everything. As you can imagine, it’s extremely freeing to have solid funding for seven years. It means I can run my lab the way I want. I’ve been able to buy new advanced equipment, hire a professional lab manager, take on more support staff.
Interestingly — and this was a surprise — the HHMI grant also prompted me to go very deep into my heritage. After the grant was announced, I began hearing from people, many of them young Native students, asking what it was like to be a Native American working in science.
I think they saw my name on the list of Investigators and then reached out to me. I’ve tried to respond and do some mentoring. But their inquiries also pushed me to learn more of my own backstory.
What did you know — or not know — about your heritage?
I grew up knowing I was biracial. I was told I was a quarter Native American.
But my relationship to my heritage was complicated. It’s a sadness to me that I didn’t know more about it when I was a child. My mom, who is white, was very young when she had me. She and my dad got divorced before I was a year old. Afterward, we moved around a lot: Arizona, Nevada, Arkansas.
My father was a Ph.D. engineer in New Mexico. Though I saw him often, when we were together we didn’t much discuss our heritage. He wasn’t all that connected to his own father. He’d been raised in Arkansas, and his father, my paternal grandfather, lived in California.
In my early 20s, I moved to California for graduate school, and that’s when my father connected me to his father and the Red Horses. My grandfather, whom I am really close to now, had a wild youth. When he finally settled down, he got a doctorate in educational administration. He directed American Indian studies programs at UCLA, Arizona State and the University of Minnesota in Duluth where he was a dean.
My grandfather also told me what he knew about our family. His father, my great-grandfather, was an orphaned Cherokee from Oklahoma. He had relocated to the Bay Area and lived among the Native peoples there. From contemporaneous newspaper reports, I’ve learned that my great-grandfather was an advocate for the Native community, fighting for their civil rights.
Introduction
Your family defies the stereotypes.
Yes, it’s interesting: I didn’t grow up living with my dad, and I don’t think he even met his dad until he was 18. Yet all three of us have doctorates!
Extreme determination seems to be a Red Horse trait. My great-grandfather, who died around the time I was born, had a lot of children with different women. I’ve met some of them. They are full of energy and determination. Me, I’m very shy, but I have this crazy drive. As a child, I wondered where that came from. Then I met the Red Horses. We’re all like that!
Did you always want to be a scientist?
I’d say that as a kid, my ambitions were unfocused. That might be because we moved around so much. I was socially awkward. I spent a lot of time alone.
Science became my passion in high school. We were living in Arkansas then. My high school biology teacher, Ms. Parnell, she lighted the science fire. One great teacher can do that.
Later, as an undergraduate at the University of Arkansas, I took an immunology course, and I performed so well that the instructor said, “Kristy, you could do lab work.”
I was like, “What’s that?”
Then I was sent to work on a study where I fed baby chicks a food additive to see if it ramped up their immune system. I’d take the chicks’ blood and count their immune cells. This was so exciting for me. It completely hooked me on research.
How did you choose a graduate school?
Well, you know, at the University of Arkansas, they weren’t very good in counseling. I had strong grades and great enthusiasm, and I applied to a whole bunch of doctoral programs. I didn’t get into any.
What ultimately happened was that San Francisco State had a master’s program aimed at bringing underrepresented people into science. I think they saw my name and must have thought, “This is someone we want.”
Do you think of yourself as someone who benefited from affirmative action?
Absolutely. And today, as the head of my own laboratory, I try to pay it back by encouraging students from underrepresented groups. I have three Native students working in my lab right now, which is extraordinarily rare at Stanford University and similar institutions.
How do you feel when you hear about attacks on affirmative action programs?
It troubles me because they’re saying that underrepresented people are getting something unearned.
When you think about it, the standards for minorities in the sciences are probably higher. To work in science, you have to rise above a lot of failures because you are testing hypotheses that may not be true. At the same time, you are sometimes encountering people questioning the validity of your even being there. To persist in that atmosphere, you need a lot of extra grit.
Introduction
How did you finally get to do a doctorate?
While I was at San Francisco State, Susan Fisher, who was studying the placenta at the University of California, San Francisco, came over to tell us about her work.
She’s an awesome science communicator. She mesmerized us by telling us how the placenta is this wild and crazy organ that does all these amazing things. I immediately asked if I could do my master’s research in her lab, and she said yes.
After completing my master’s, I stayed on at UCSF to do my doctorate with her. We worked on placental development and how fetal placentas connect to the mother’s blood supply during pregnancy. We found that certain specific guidance proteins direct placental cells to arteries rather than to veins, and we published several papers together.
Did your placenta research lay the groundwork for your cardiac studies?
Absolutely. There’s a straight line from our studies of the placenta to our current work on blood vessels.
That’s because when cells leave the placenta and migrate into the mother’s uterus, they home in on the arteries — not the veins, but specifically the arteries. And then they line the arteries and make their own little placenta-derived blood vessels. Those redirect the blood flow from the mother’s uterus into the placental spaces so that the fetus can absorb oxygen and nutrients.
This all has to do with blood vessels, right? They’re mimicking a blood vessel, and they’re going in to co-opt a blood vessel and form a little conduit.
So yeah, studying the placenta is how I got interested in blood vessels and the different molecules that pattern them.
How close are you to finding a regenerative therapy for heart attacks?
It’s impossible to predict. But I’d say we’re 10 to 20 years away. Right now, two-thirds of my lab is studying regeneration.
In mice we’ve shown that the biochemical pathways we’re studying can improve recovery after an experimental heart attack. That’s a first step toward it potentially working in humans. But I’m really interested in using different species to learn new things about the collateral blood vessels.
Guinea pigs, for instance, are the only species that have perfectly performing collateral arteries in their hearts. That is, their collaterals can completely reroute the blood flow after any blockage in the coronary arteries, so there’s no cardiac muscle death. They have collateral arteries throughout their lives, not just as a consequence of heart injuries. Because of this, guinea pigs are essentially heart-attack proof.
We’re asking how guinea pig development is different so that we can discover the molecules that make the collaterals form in their heart. We hope this will result in applications in other species. We’d like to transfer this feature to mice and eventually humans.
Twenty years? That’s a long time to wait for something concrete to happen.
It’s OK with me because a lot of the fun stuff happens along the way. That’s why one becomes a scientist in the first place. You get to be a detective and an artist. You put clues together. And then you learn how an organ works.
- SEO Powered Content & PR Distribution. Get Amplified Today.
- Platoblockchain. Web3 Metaverse Intelligence. Knowledge Amplified. Access Here.
- Source: https://www.quantamagazine.org/she-studies-growing-arteries-to-aid-heart-attack-recovery-20230213/
- $9 million
- 000
- 10
- 20 years
- 2021
- a
- Able
- About
- about IT
- above
- Act
- Action
- actually
- administration
- Adult
- adults
- advanced
- advocacy
- advocate
- After
- Aid
- All
- alone
- always
- amazing
- ambitions
- American
- among
- and
- animals
- announced
- Anticipated
- applications
- applied
- appointed
- approach
- AREA
- arizona
- arkansas
- around
- artist
- Associate
- Atmosphere
- attack
- Attacks
- Baby
- back
- Backup
- Bay
- Beach
- because
- become
- becomes
- before
- began
- being
- Big
- biology
- blocked
- Blocks
- blood
- body
- born
- bring
- Bringing
- Brings
- brought
- Bunch
- buy
- california
- called
- Calls
- carry
- cases
- Cells
- centered
- certain
- Chamber
- change
- child
- Children
- Choose
- circles
- Civil Rights
- clarity
- Close
- Collateral
- colleague
- colleagues
- color
- come
- community
- completely
- completing
- complicated
- Confirm
- Connect
- connected
- Connections
- contains
- conventional
- converge
- could
- Couple
- course
- covering
- created
- crucial
- Current
- Dad
- Death
- deep
- describe
- described
- details
- determination
- develop
- Development
- develops
- DID
- Die
- died
- different
- direct
- discover
- discovered
- discuss
- Disease
- Dont
- double
- down
- drive
- during
- Early
- easily
- educational
- Effective
- efficiency
- efficient
- efficiently
- effort
- emerging
- encountering
- encouraging
- energy
- engineer
- enthusiasm
- Entire
- entirely
- equipment
- essentially
- estimated
- Even
- eventually
- EVER
- Every
- everything
- exciting
- existing
- Expand
- expanded
- expansion
- extend
- extra
- extraordinarily
- extremely
- Failure
- family
- fascinating
- faster
- Feature
- Fed
- few
- fighting
- fill
- Finally
- Find
- finding
- Fire
- First
- flow
- focusing
- food
- form
- formation
- formed
- found
- Francisco
- from
- full
- fun
- functions
- fund
- funding
- future
- gap
- generate
- get
- getting
- given
- gives
- Go
- Goes
- going
- good
- graduate
- grant
- great
- groundbreaking
- groundwork
- Group’s
- Grow
- Growing
- Growth
- happen
- happened
- happens
- having
- head
- Health
- hearing
- Heart
- Heart Attack
- Heart disease
- Heart Failure
- help
- heritage
- High
- higher
- hire
- Home
- Honors
- hope
- Horse
- How
- HTML
- HTTPS
- human
- Humans
- idea
- ideas
- identical
- identified
- immediately
- Immune system
- important
- impossible
- improve
- in
- In other
- Indian
- individual
- instance
- instead
- Institute
- institutions
- interested
- interesting
- interrupted
- Interviews
- Investigators
- involved
- IT
- itself
- Key
- Kid
- Kind
- Know
- Knowing
- lab
- Label
- laboratory
- Last
- leader
- LEARN
- learned
- Leave
- legendary
- Level
- Life
- Line
- List
- little
- Lives
- living
- Long
- long time
- Look
- looked
- looking
- Lot
- made
- maintenance
- make
- Making
- manager
- many
- master’s
- material
- means
- medical
- medicine
- Meet
- member
- mentoring
- Mexico
- mice
- might
- migrate
- million
- minnesota
- minorities
- modified
- molecular
- mom
- more
- move
- MS
- name
- native
- Natural
- Nature
- Need
- needs
- network
- NEVADA
- New
- New York
- next
- novel
- occurred
- oddly
- Oklahoma
- Old
- ONE
- opportunities
- optimum
- originated
- Other
- Others
- own
- Oxygen
- Paper
- papers
- passion
- Pattern
- Pay
- People
- performing
- perhaps
- period
- permanently
- physical
- pieces
- Place
- plato
- Plato Data Intelligence
- PlatoData
- please
- Point
- possibility
- potentially
- predict
- Pregnancy
- prestigious
- prevent
- prize
- probably
- process
- professional
- Professor
- Program
- Programs
- promised
- proof
- Protein
- Proteins
- Publication
- published
- pump
- pushed
- put
- Quarter
- quickly
- raised
- RARE
- reached
- real
- reason
- receive
- recovery
- Red
- redirect
- reducing
- regenerative
- regular
- relationship
- repair
- Reports
- rescue
- research
- researcher
- Respond
- response
- result
- resulting
- Revealed
- rights
- Rise
- Run
- Said
- same
- San
- San Francisco
- School
- Science
- SCIENCES
- Scientist
- scientists
- searching
- sections
- seems
- selected
- set
- Settled
- seven
- several
- shown
- Signatures
- similar
- small
- So
- socially
- solid
- some
- Someone
- something
- Sources
- spaces
- speaking
- special
- specialized
- specially
- specific
- specifically
- spent
- spread
- Staff
- standards
- stanford
- Stanford university
- Starting
- State
- stayed
- Stem
- Step
- straight
- strength
- strong
- Students
- studies
- Study
- Studying
- such
- summer
- supply
- support
- surprise
- Susan
- system
- Take
- teacher
- techniques
- Testing
- The
- The Future
- their
- therapy
- There.
- therefore
- thing
- things
- thought
- three
- Through
- throughout
- time
- to
- today
- together
- too
- tools
- top
- toward
- transfer
- transformed
- treating
- true
- two-thirds
- types
- ucla
- Ultimately
- underrepresented
- understanding
- Unexpected
- university
- University of California
- University of Minnesota
- us
- Vessel
- Video
- vital
- wait
- ways
- webp
- What
- whether
- which
- while
- white
- WHO
- Wild
- will
- wisdom
- Women
- Work
- worked
- working
- works
- would
- Wrong
- year
- years
- young
- Your
- yourself
- youth
- zephyrnet